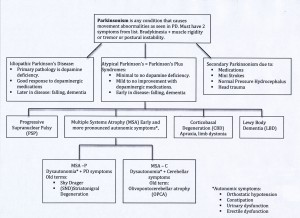
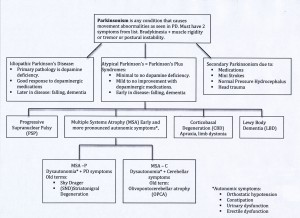
Parkinsonism is an umbrella term used for individuals who present with some of the symptoms of Parkinson’s with the main feature being slowness of movement. Idiopathic Parkinson’s disease is the most common form of Parkinsonism and the most treatable. It is typically referred to as: Parkinson’s disease or Parkinson’s or PD. The ‘Atypical Parkinson’s’ (also known as Parkinson’s Plus Syndromes) houses 4 diagnostic categories. Each category has it’s own distinguishing features. Secondary Parkinsonism is caused by something other than a lack of dopamine but can effect the dopamine system. An example of a secondary Parkinsonism is the result of medications which block the action of dopamine. This type of secondary Parkinsonism can be reversible by removing the medication causing the symptoms.
When someone is diagnosed with Parkinsonism there is often uncertainty what that means. ‘Does that mean I have Parkinson’s disease?’ You may, or you may have something else that currently looks like Parkinson’s but over time your symptoms will become more clear. Also, your response to Parkinson’s medications will offer more information to help with a more definitive diagnosis. This process can take some time to unfold depending on how pronounced the individual symptoms present themselves and if medications offer substantial relief or not. Click on the chart to see a larger version.
As you look at the chart, the terms falling and dementia can be disconcerting. When looking at information which condenses an entire diagnoses in a few words, you should view it with caution since the degree which an individual can experience symptoms is largely variable and not everyone experiences all symptoms. The autonomic symptoms experienced by the ‘Atypical Parkinson’s’ category may also effect people with PD but to a lesser degree and only contributes to the sometimes daunting task of establishing a definitive diagnosis. A Movement Disorder neurologist is the most knowledgeable in sorting out Parkinsonisms.